Bringing Our RA Experiences Together - Results from the 2019 RA In America Survey
Life with rheumatoid arthritis (RA) can often feel lonely, especially when we are misunderstood by friends, family, and even healthcare providers. As isolating as RA can be, you are not alone in your RA journey. In fact, more than 3,700 were eager to share what they have experienced in living with RA in our 2019 Rheumatoid Arthritis In America Survey.
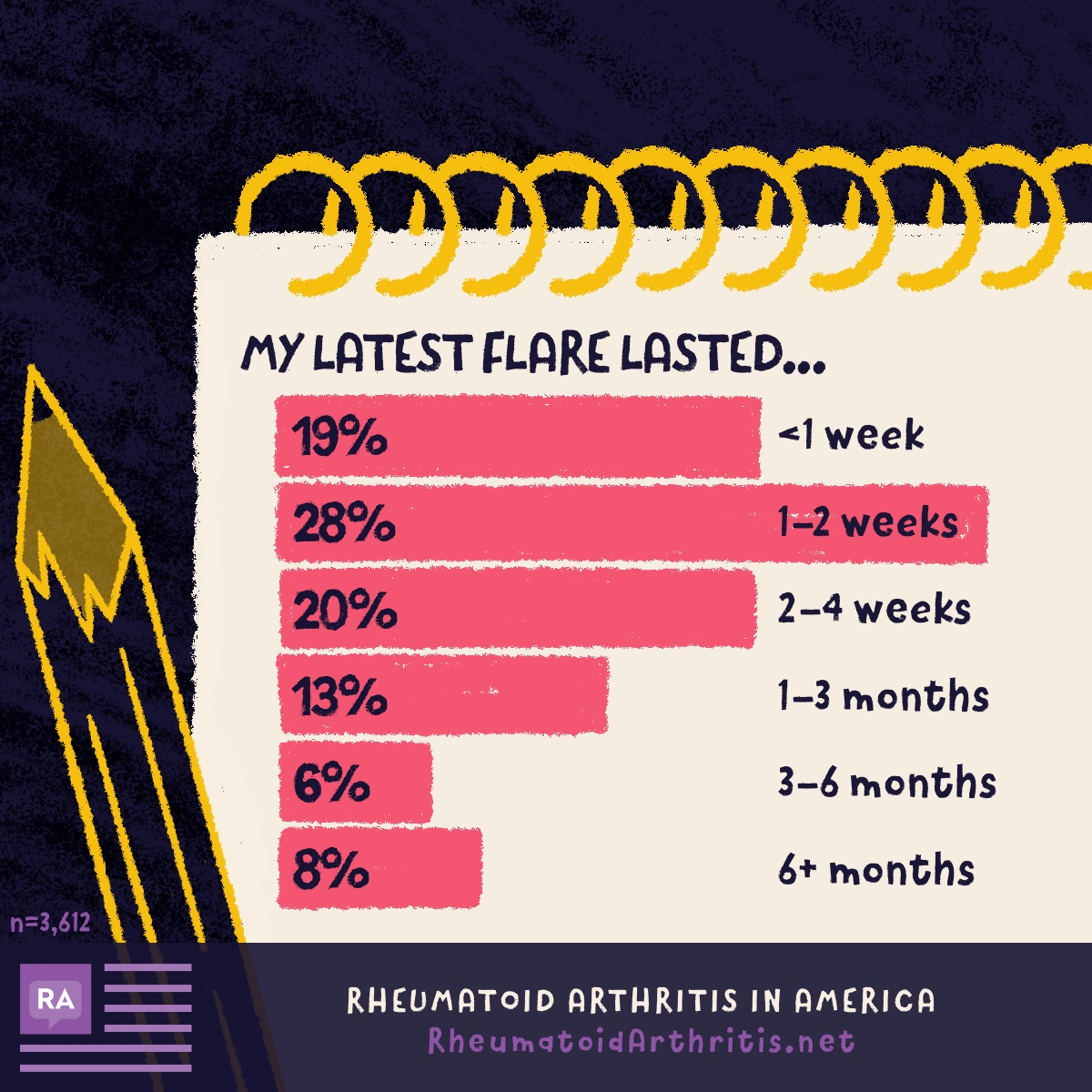
How long can an RA flare last?
Rheumatoid arthritis is a condition that often affects each person differently. When asked to describe the overall severity of their RA, over 60 percent of individuals reported having moderate RA. Over the last year, 30 percent of respondents experienced 2-4 flares, and 25 percent experienced more than 10 flares.
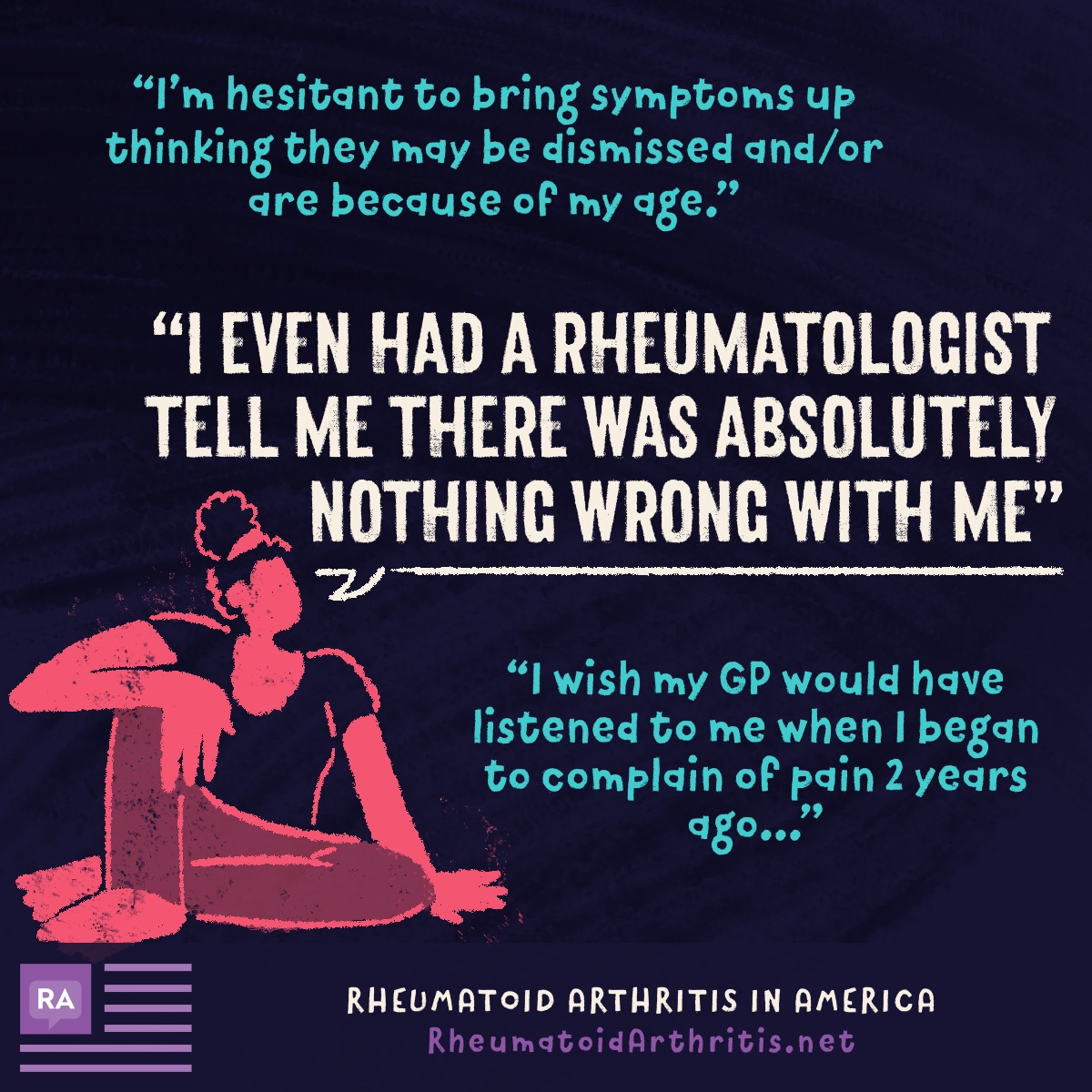
Misdiagnosis and being misunderstood by healthcare professionals
Before receiving their RA diagnosis, 43 percent of respondents were first misdiagnosed. Although 22 percent received an RA diagnosis after seeing one healthcare professional, 44 percent saw 3 or more healthcare professionals to obtains an RA diagnosis.
Impact of RA on mental health and well-being
The symptoms of rheumatoid arthritis can negatively impact mental health and overall wellbeing. 92 percent of respondents experienced fatigue, a symptom that impacts the ability to carry out everyday tasks and activities. More than half experienced anxiety and depression. Similarly, 61% experienced brain fog and other types of cognitive impairment.
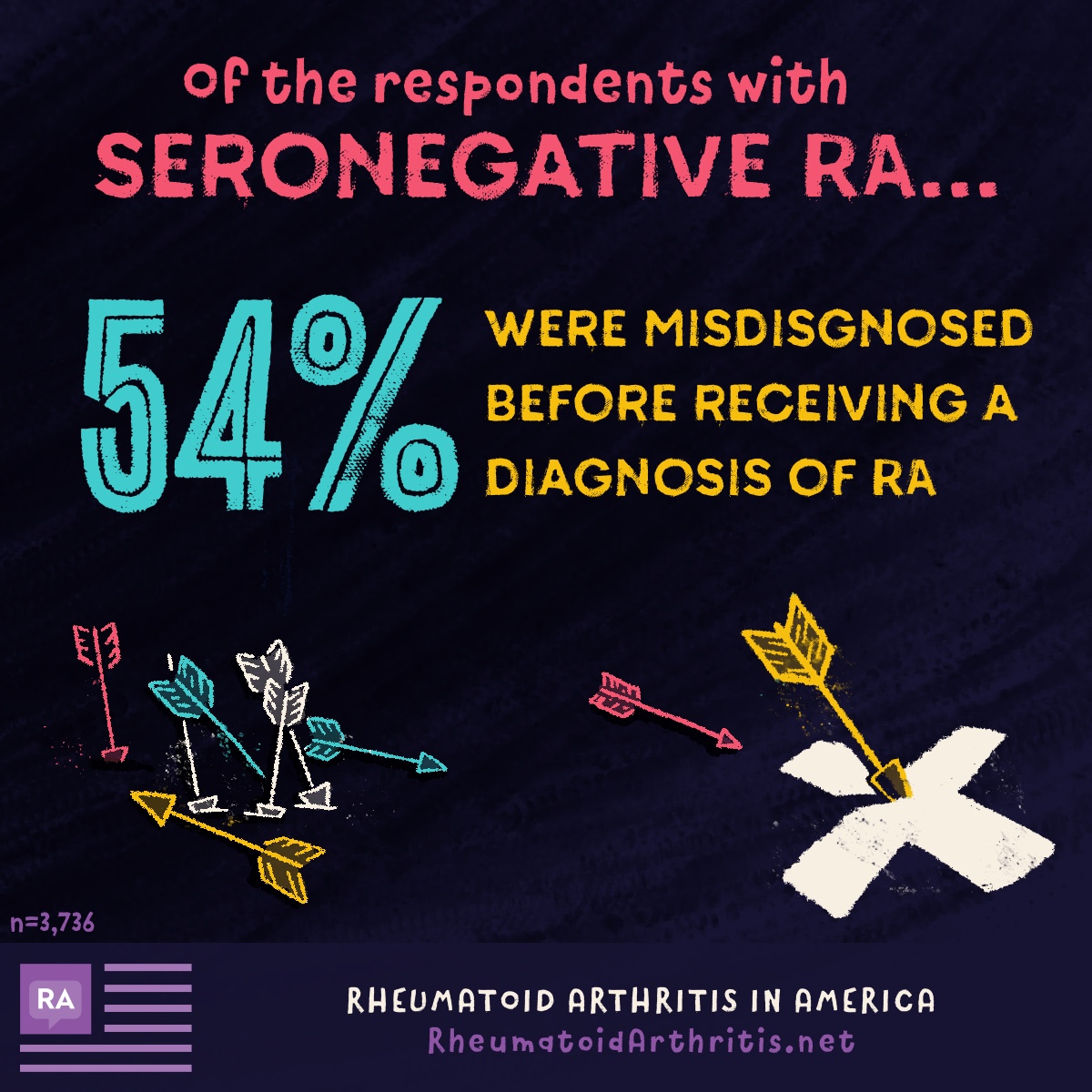
Differences in RA diagnosis experience for seronegative RA patients
Blood tests are an important part of attaining an RA diagnosis. Certain substances are found in the blood of people living with RA that may suggest inflammation. However, blood tests do not always paint a clear picture of RA. This is especially true for those who have been diagnosed with seronegative RA.
Many members of the community have shared how difficult it is to receive a diagnosis of RA. 43 percent of the total respondents were initially misdiagnosed when receiving an RA diagnosis. Misdiagnoses in patients with seronegative RA were as follows:
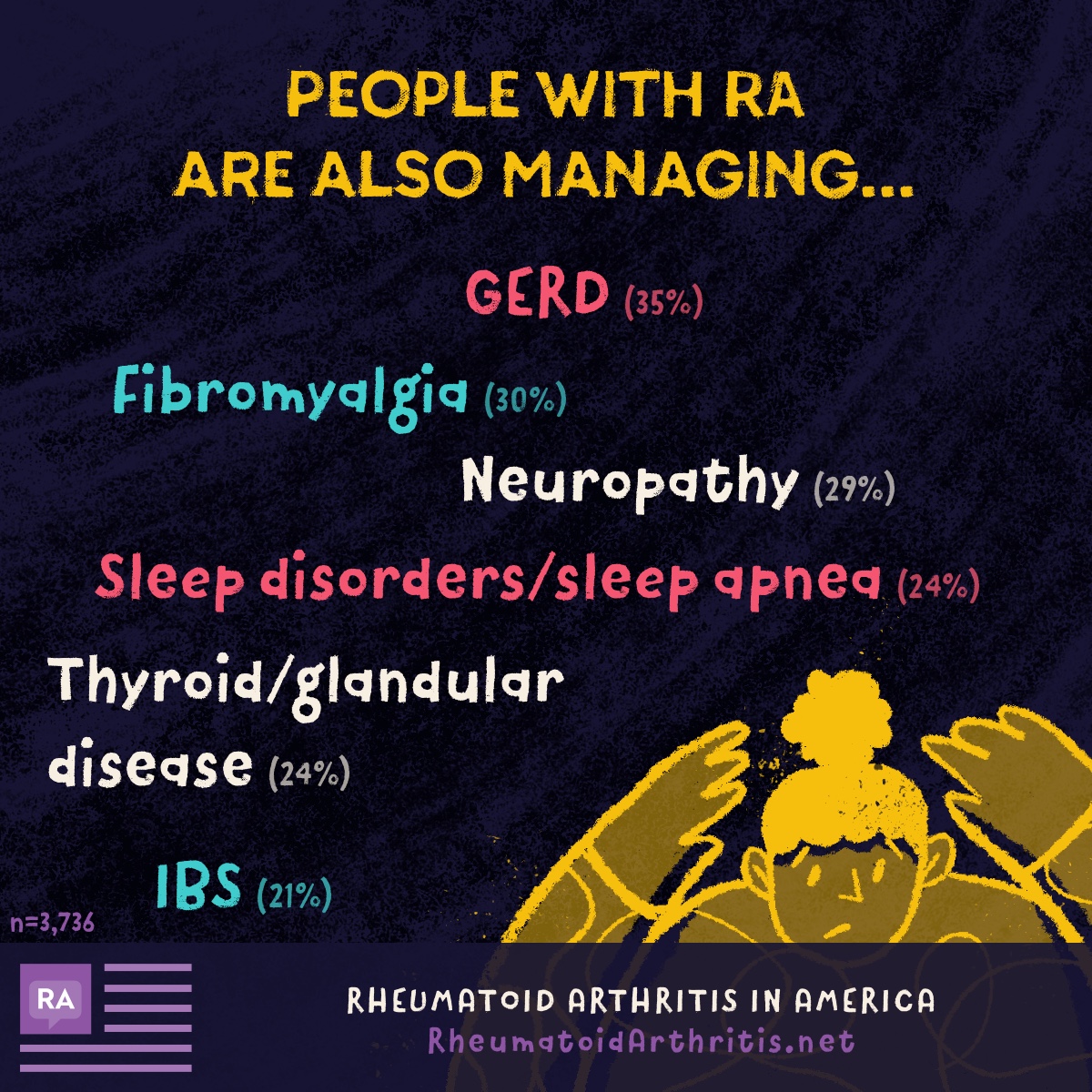
Managing other conditions in addition to RA
Many individuals living with rheumatoid arthritis are also managing other health conditions. In some cases, these conditions were complications or manifestations of RA, as the autoimmune condition affects more than just joints and bones.
We will continue to provide support!
Although rheumatoid arthritis can often leave us feeling isolated, results from our 2019 Rheumatoid Arthritis In America Survey shows that we are not alone. There is power in talking about our symptoms. There is power in sharing stories about our rheumatoid arthritis journey. RheumatoidArthrits.net will continue to be an online community of information and support for this living with RA.
The RA In America 2019 Survey was conducted online from June through September of 2019. A total of 3736 people completed the survey.
Join the conversation