Why Are RA Drugs So Expensive?
A recent report noted that prescription drug prices rose 13 percent last year. Most of the increase in costs is attributed to specialty drugs designed to treat chronic conditions.1
Rheumatoid arthritis drugs, primarily biologic medicines, represent specialty drugs with high costs.
The cost of specialty drugs
While only representing 1 percent of the prescriptions filled, specialty drugs accounted for 31 percent of the total costs of medicines. 1
In fact, the largest increase in healthcare prices over the past few years has been in pharmaceuticals. This is even prompting a war between insurance companies and pharmaceutical companies.2,3
Why are RA biologics so expensive?
I’ve been on numerous biologic medications to treat rheumatoid arthritis. I’m thankful for these complex drugs - it’s clear that they slowed disease progression. I’m currently taking Rituxan.
After a recent infusion, my insurance company sent an explanation of benefits (EOB) form showing the cost and coverage of the medicine and infusion services (see a photo of the form).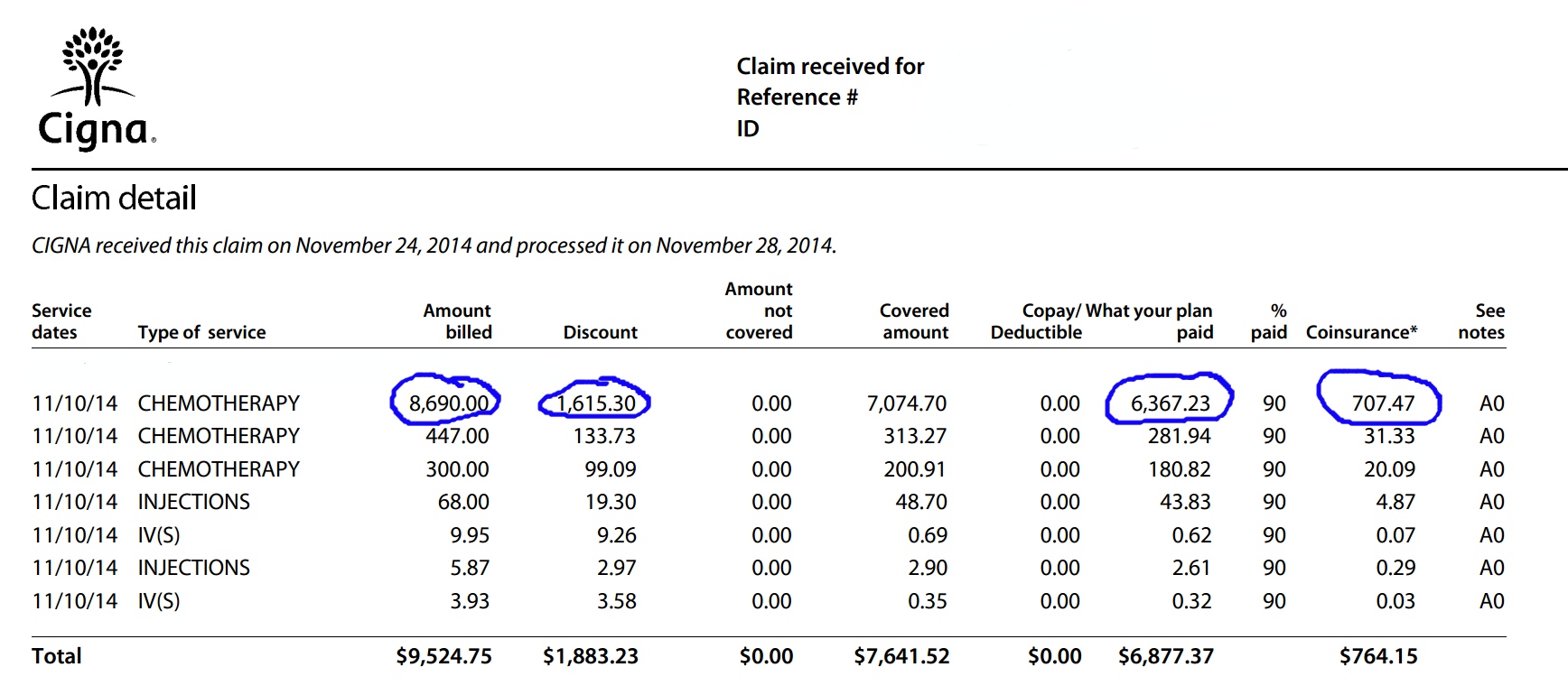
Cost, price structures, and mark-ups
The form shows that the charges billed by the infusion clinic for the Rituxan was $8,690 for 1,000 mg of medicine. I’m curious about the source of this cost and can only assume that this is the cost suggested by the drug manufacturer - sort of like a “suggested retail price.”
The adjustments made by the clinic were for $1,615 making the final cost of the drug that the insurance company agreed to pay $6,367. The mark-up on Rituxan must be huge if the adjustment was that much less than the original cost.
Insurance companies obviously know the price structures of medicines and know what price pharmaceutical companies and clinics will actually accept in order to cover their costs. Price structures for medical treatments are individually negotiated between insurance companies and hospitals/clinics.
My clinic also charged for the infusion that included the nurse and equipment and for other pre-medication drugs like solu-medrol and Benadryl. The total cost of this infusion procedure was $7,641.
Out-of-pocket costs for infusions
My out-of-pocket costs were $764 due to co-pays and deductibles. Fortunately, Genentech, the manufacturer of Rituxan, provides a co-pay assistance plan and they covered $702 to help cover the costs.
I receive 8 Rituxan infusions a year making a total annual cost of such treatments $61,128. And that does not include other costs associated with my RA treatment including other medicines, doctor visits, blood tests, imaging, and surgeries.
Costs are passed on to the patient
Biological medicines are understandably expensive because of the research, development, and complex manufacturing processes involved. Such medicines also have extended patent protection over chemical pharmaceuticals in order to help drug companies recoup the extensive costs. Those costs are passed on to the patient.
The wild difference in charged costs versus covered costs as shown on the EOB can only make one wonder about drug company profit margins. Clearly, biologics are big business. In 2010, Amgen’s Enbrel had over $3 billion in sales just in the United States. This represented 23 percent of Amgen’s annual sales.4
Will biosimilars bring a lower cost?
Four RA drugs - Humira, Enbrel, Remicade, and Rituxan – are among the top-selling biologics in the United States. And these biologics will lose their patent protection soon.5
This is the reason that so-called "biosimilars", generic equivalents for biologics, are being developed and will soon be approved for patient use.
The real cost of Rituxan isn’t a mystery that I will likely solve any time soon. There are numerous pharmaceutical, insurance, healthcare system, and political players involved. But one has to avoid skepticism driving you to not take prescribed medicines that can help slow the disease progression.
While issues of costs and insurance reimbursements need to be addressed, right now, I’m just thankful for a medicine to treat RA, insurance coverage, and co-pay coverage by the pharmaceutical company.
Community Poll
What flare symptom do you wish you could avoid the most?
Join the conversation