RA in America 2015
The RA In America 2015 online survey was conducted learn about life with rheumatoid arthritis (RA) from over 3,100 individuals who are living with RA. The 2015 survey continued to build upon the findings from previous surveys, illustrating the effect RA has on one’s life:
- Obtaining an RA diagnosis is not often straightforward and timely for most, rather it is a process involving
multiple healthcare professionals, office visits and diagnostic tests - With fatigue being the most common symptom reported, as well as many being impacted by joint pain and
stiffness throughout the day, its not surprising that all facets of respondents’ lives have been impacted by
RA - Respondents reported playing an active role in making treatment decisions, however most turned to their
healthcare provider as a resource, as well as depending on their recommendations for starting and
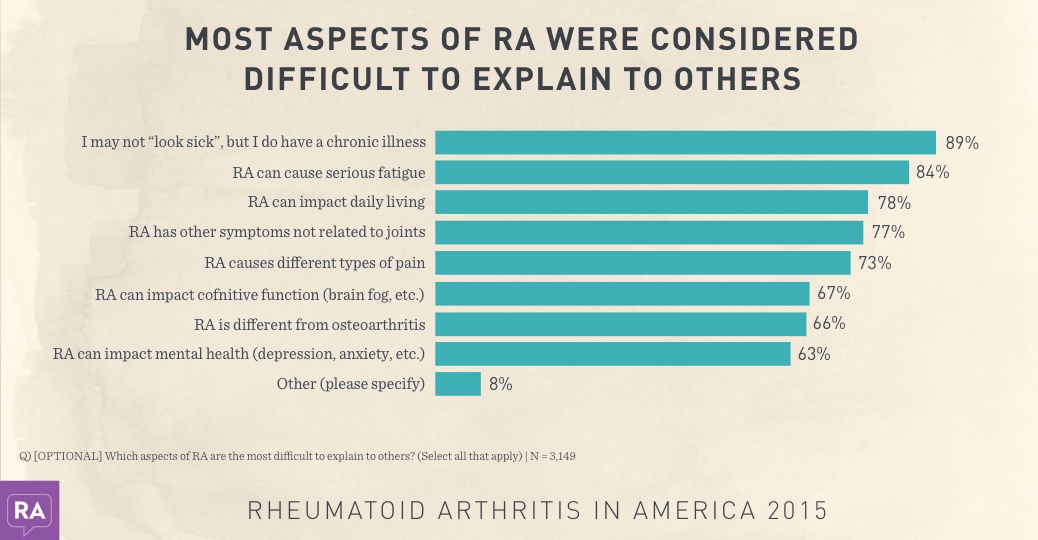
selecting medications - RA is thought to be widely misunderstood by those not affected by the disease
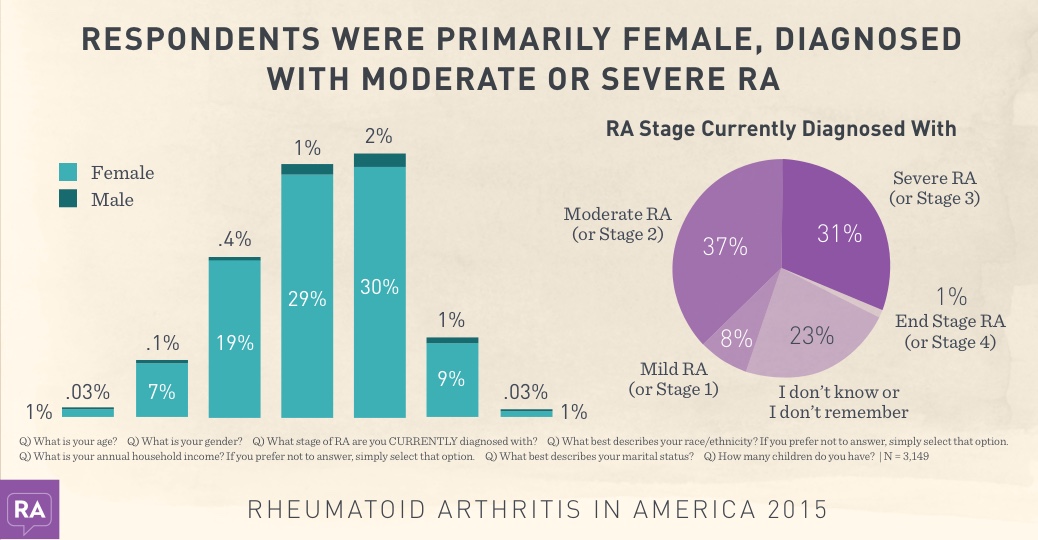
Most respondents were Caucasian and from
households with less than $100K annual income,
as well as being were married (68%) and having
children (83%). 14% were separated/divorced
and 6% were never married.
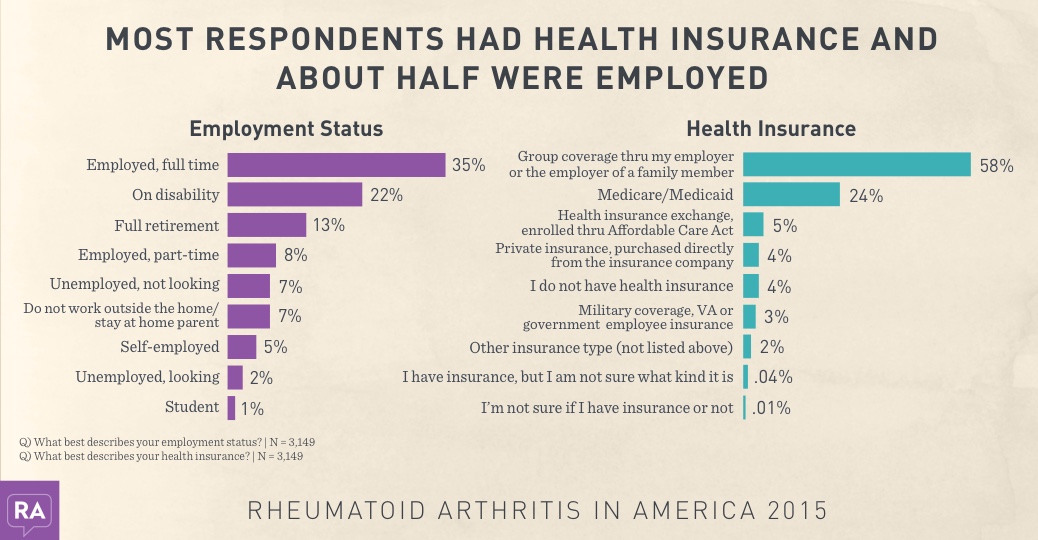
48% of respondents were employed in some
capacity and 22% were on disability. Incidence of
those not having health insurance has decreased
this year, potentially due to the Affordable Care
Act.
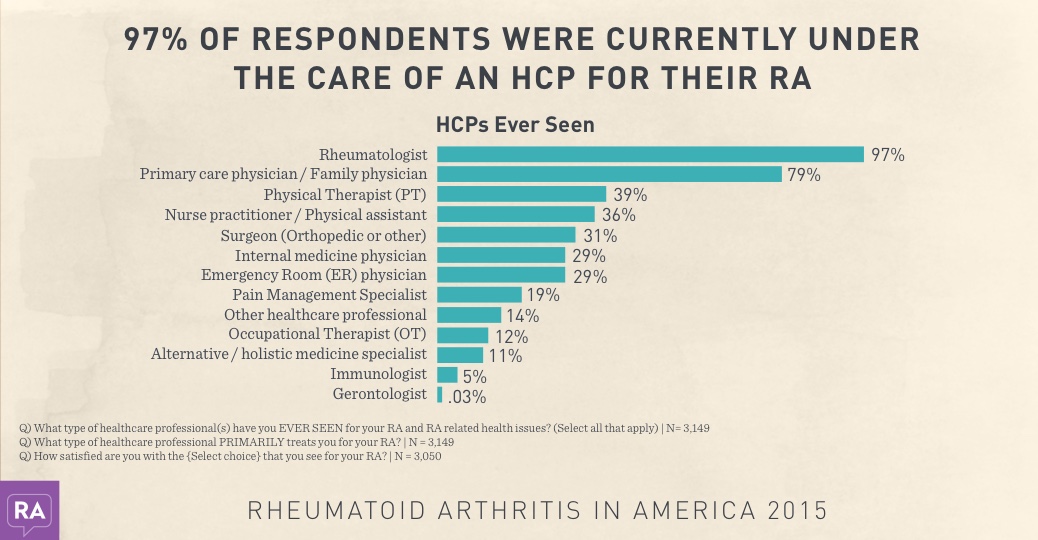
97% of respondents were seen by a
rheumatologist for their RA, and 79% were seen
by a primary care or family physician.
39% sought care from a physical therapist and
only 12% were seen by an occupational therapist.
Almost ¾ of respondents satisfied with the HCP
they currently were seeing for their RA.
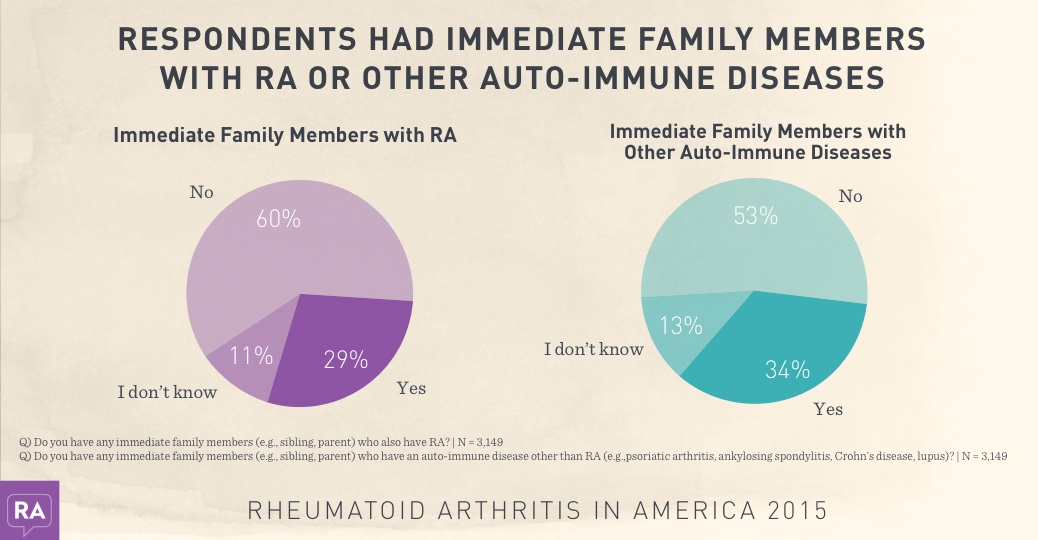
And a little over a third of respondents had
immediate family members who had another
type of auto-immune disease, and 29% had a
family member with RA.
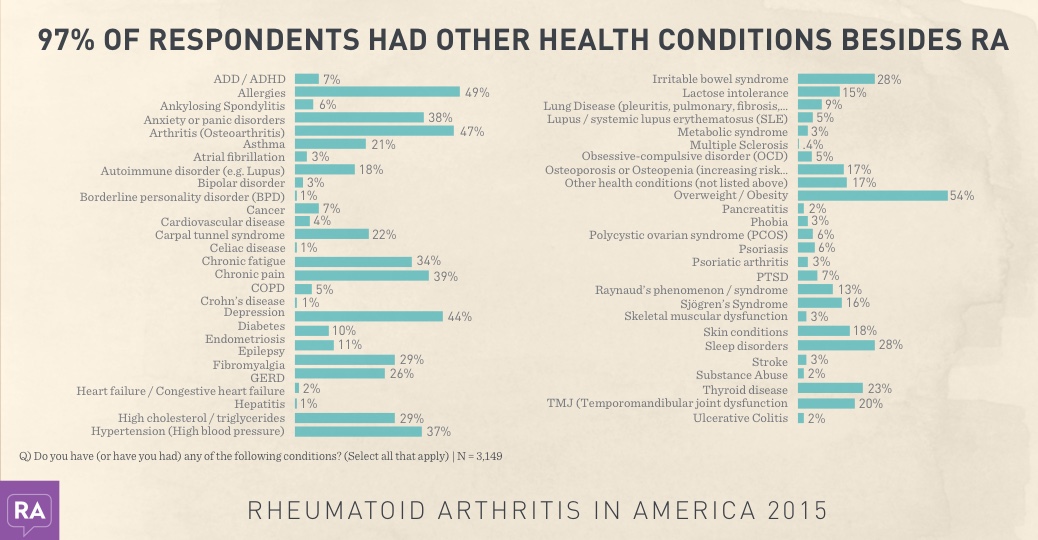
Obesity, allergies, arthritis and depression were
among the leading additional health conditions
reported by respondents.
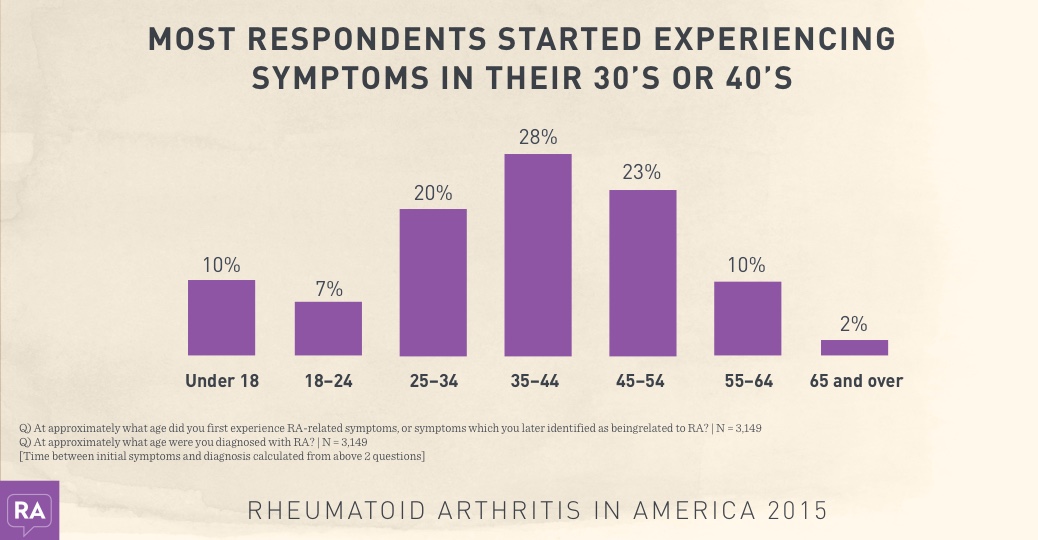
One-third of respondents were formally
diagnosed within a year of experiencing
symptoms, with 29% diagnosed between 35-44
years of age and 28% diagnosed between 45-54.
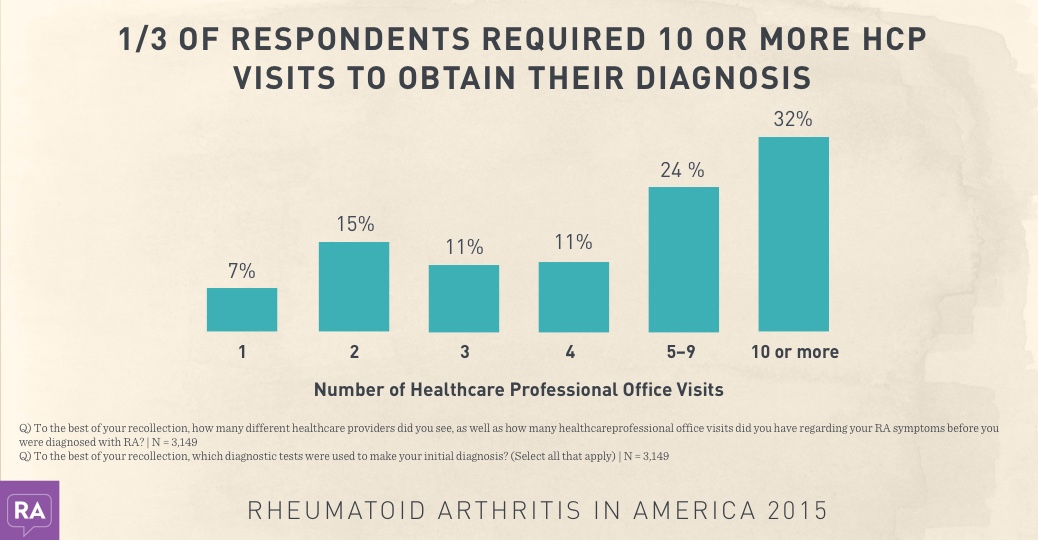
55% of respondents saw 2-3 healthcare
professionals to obtain their RA diagnosis. The
Rheumatoid Factor test was most commonly
used as a diagnostic tool (80%), followed by
Complete Blood Count (73%) and physical
examination (72%). On average, more than 5
diagnostic tests were employed to make a
diagnosis.
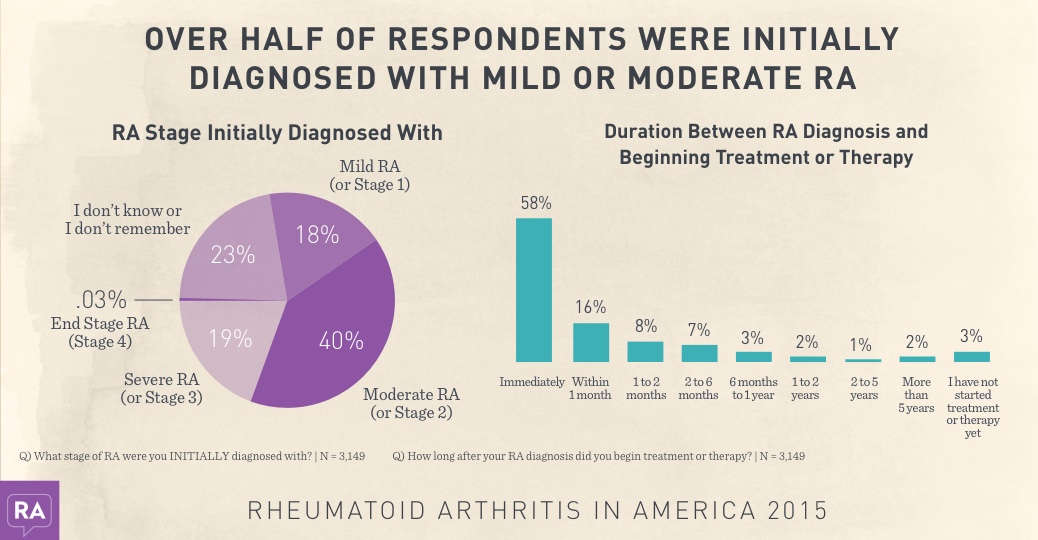
A majority of respondents started treatment
immediately after diagnosis.
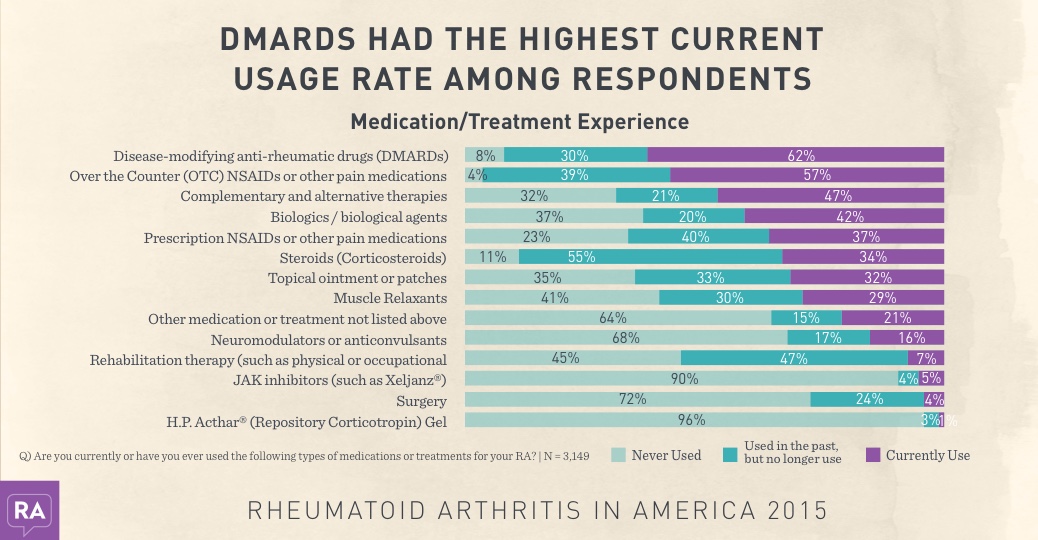
Methotrexate had both the highest usage and
abandonment rate of DMARDs (46% and 45%
respectively).
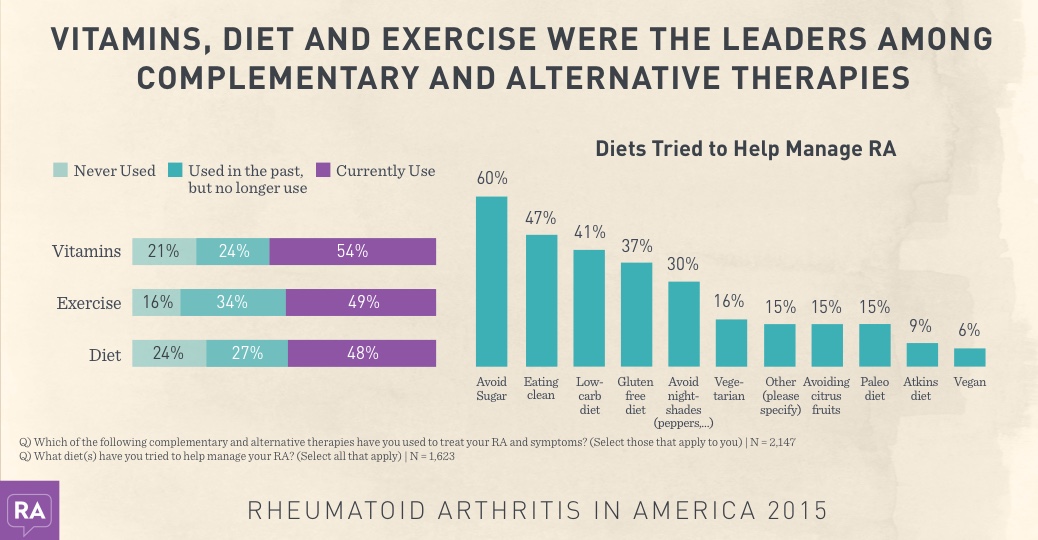
Avoiding sugar and eating clean were diets
frequently tried by respondents to help manage
their RA, as well as low-carb diets and gluten
free.
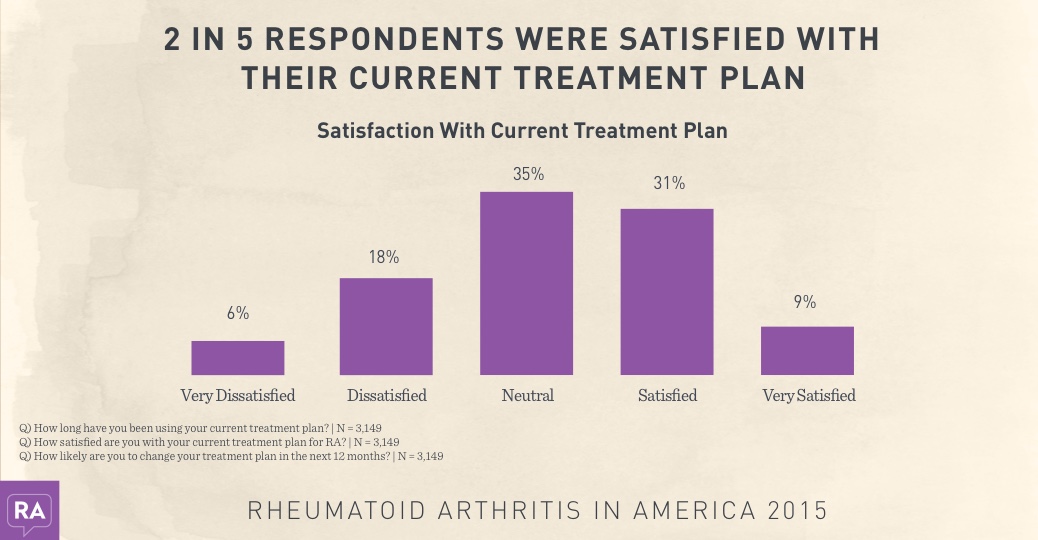
Most respondents had been on their current
treatment plan less than 2 years and 43% were
likely to change their treatment plan within the
next year.
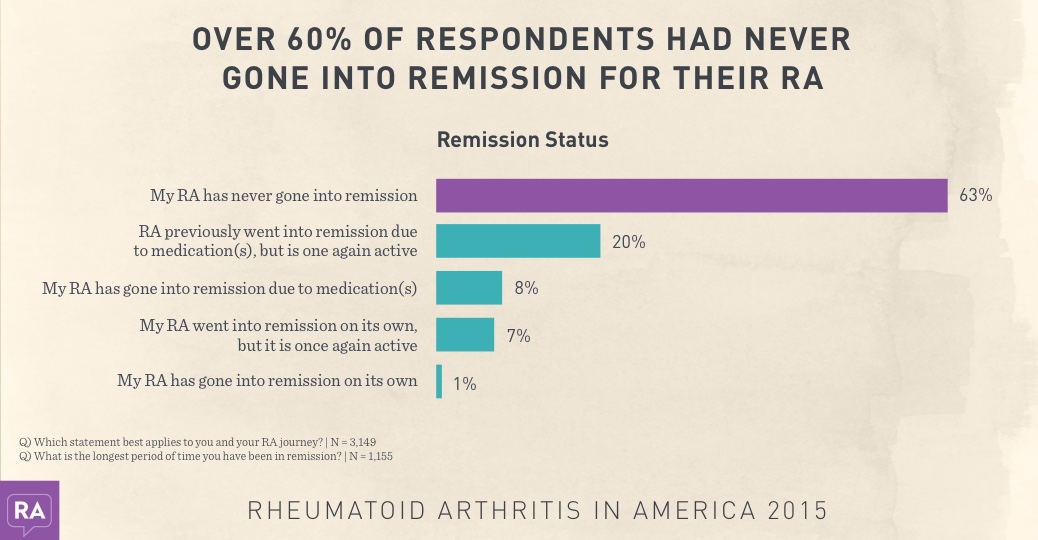
Of those who had gone into remission, it was
typically due to medication. For 42% of
respondents, remission lasted less than 6
months. Another 22% experienced remission for
6-11 months.
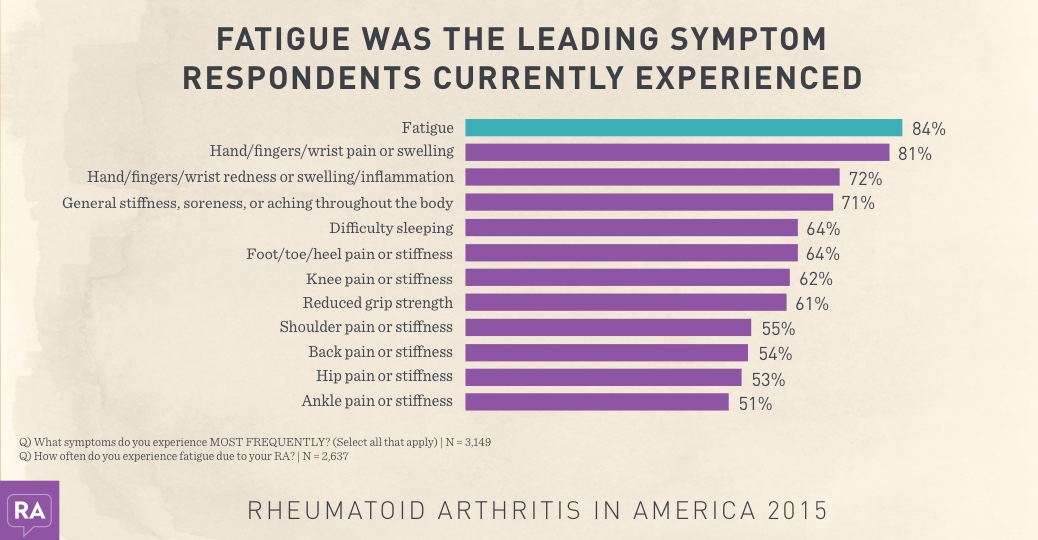
Respondents experienced an average of 15.5
symptoms and fatigue was experienced on a
daily basis for 73% of its sufferers. Less than 1%
of respondents were not experiencing RA
symptoms at the time of the survey.
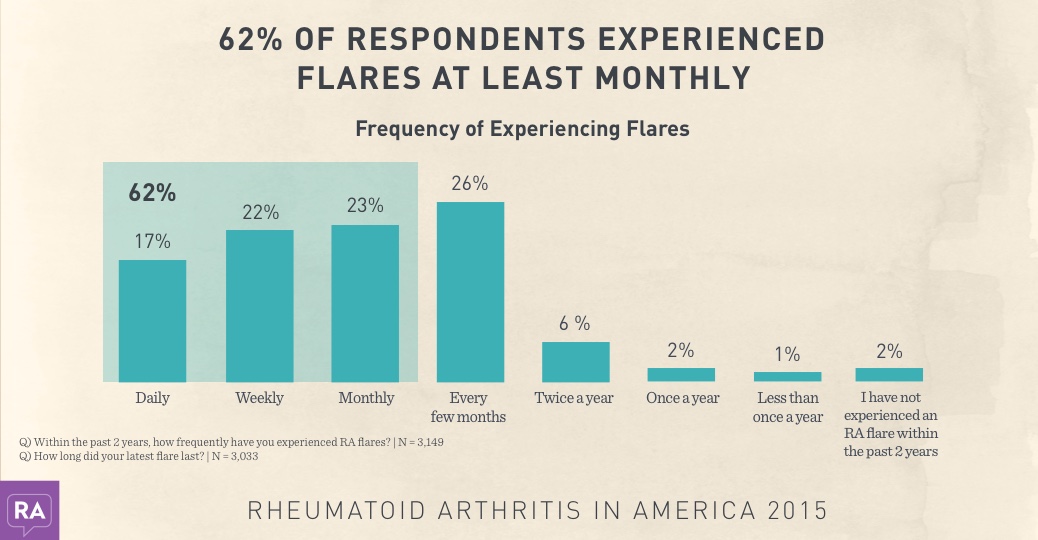
Almost 1 in 4 experienced flares on a weekly
basis. For over half of respondents, their latest
flare latest no longer than 2 weeks.
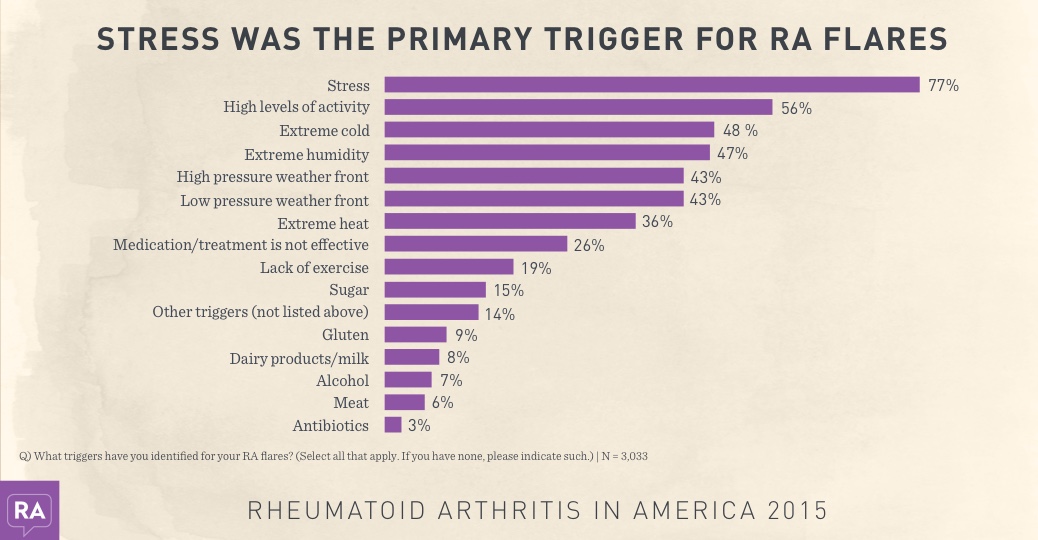
11% of respondents have not identified any
triggers for their RA flares. Of those with triggers
for their flares, they had 4.2 triggers on average.
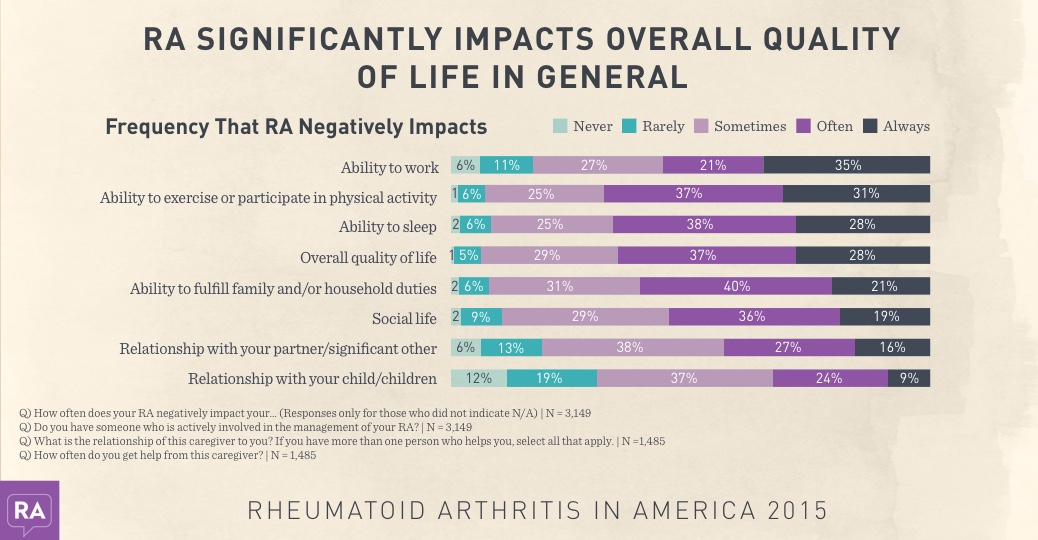
RA most negatively impacts one’s ability to work,
participate in physical activity, sleep, and their
overall quality of life. 47% of respondents had a
caregiver to help manage household or health
related responsibilities; typically a spouse who
helped them daily.
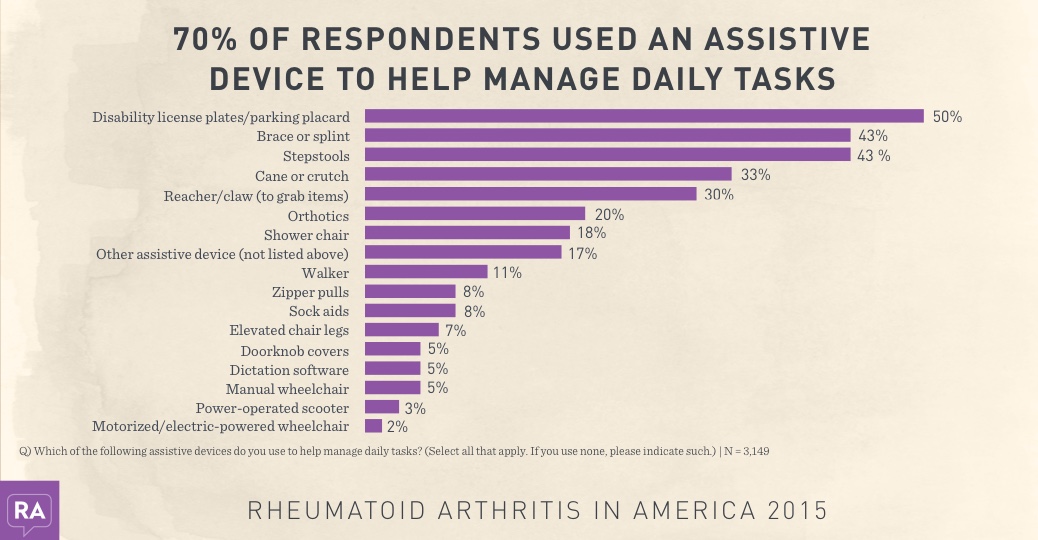
Assistive device users employed an average of
3.1 devices. Half of assistive device users had
disability license plates/placards, whereas
wheelchairs and scooters were employed by less
than 10%.
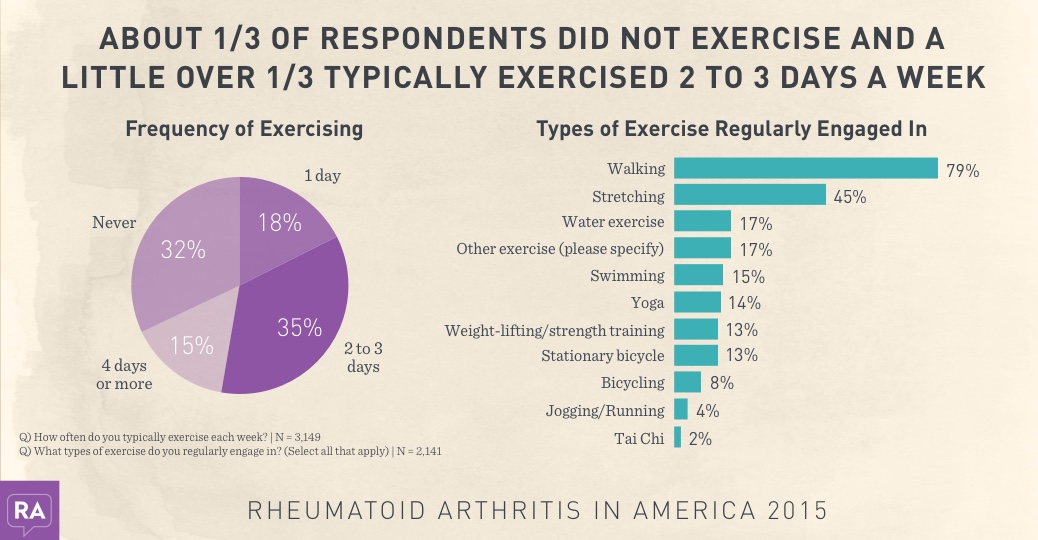
RA symptoms, including fatigue, were cited as
the leading barrier to exercising, followed by
motivation.
Join the conversation